Craniotomy vs. Craniectomy: A Detailed Comparison of Brain Surgery Procedures
When facing the prospect of brain surgery, understanding the nuances between different procedures is crucial for both patients and their families. Two common procedures, craniotomy and craniectomy, often cause confusion due to their similar-sounding names and shared purpose: accessing the brain. However, they are distinct surgical interventions with different techniques, applications, and potential outcomes. This comprehensive guide will delve into the intricacies of craniotomy vs. craniectomy, providing a clear understanding of their differences, benefits, and the circumstances under which each procedure is preferred.
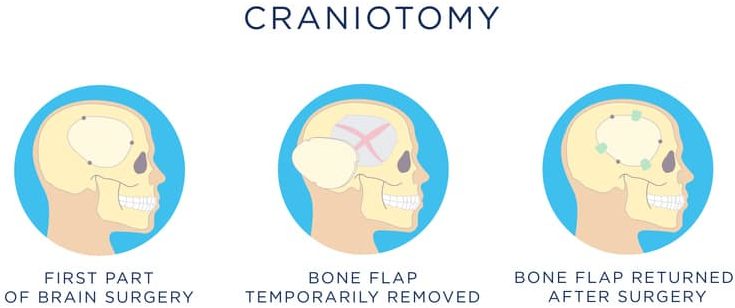
Craniotomy: A Precise Approach to Brain Access
A craniotomy involves temporarily removing a section of the skull, called a bone flap, to access the brain. The bone flap is carefully preserved and, after the surgical procedure on the brain is completed, meticulously secured back into its original position using plates, screws, or sutures. Think of it like opening a door to access a room, then carefully closing and securing the door after you’re done. This ability to restore the skull to its original form is a defining characteristic of a craniotomy.
The Craniotomy Procedure: Step-by-Step
- Preparation: The patient is placed under general anesthesia, and the surgical site is prepped and sterilized. Image guidance systems (like MRI or CT scans) are often used to precisely map the location for the incision.
- Incision and Flap Creation: A surgical incision is made in the scalp, and the soft tissues are carefully retracted to expose the skull. Using specialized surgical tools, a section of the skull is precisely cut and removed as a single bone flap.
- Brain Access and Intervention: With the brain now accessible, the neurosurgeon performs the necessary procedure, which could involve tumor removal, aneurysm clipping, hematoma evacuation, or other interventions.
- Closure: Once the brain surgery is complete, the bone flap is carefully repositioned and secured to the skull using titanium plates and screws or sutures. The scalp and soft tissues are then closed in layers.
When is a Craniotomy the Preferred Choice?
Craniotomies are typically performed when the brain swelling is not anticipated to be a significant issue post-surgery. It is often the preferred approach for:
- Tumor Resection: Removing brain tumors, both benign and malignant.
- Aneurysm Clipping: Clipping or coiling brain aneurysms to prevent rupture.
- Hematoma Evacuation: Removing blood clots (hematomas) from the brain.
- Abscess Drainage: Draining brain abscesses.
- Seizure Surgery: Resecting brain tissue causing seizures.
- Vascular Malformations: Addressing arteriovenous malformations (AVMs).
Craniectomy: Decompressive Surgery for Brain Swelling
In contrast to a craniotomy, a craniectomy involves removing a portion of the skull and not immediately replacing it. The bone flap is typically stored in the patient’s abdomen (to keep it sterile and alive) or cryopreserved for later re-implantation. This creates more space for the brain to swell without being compressed, which can be life-saving in cases of severe brain injury or swelling. The missing section of the skull is replaced in a subsequent procedure called a cranioplasty, typically several weeks or months later, once the swelling has subsided.
The Craniectomy Procedure: Managing Increased Intracranial Pressure
- Preparation: As with a craniotomy, the patient undergoes general anesthesia, and the surgical site is prepared.
- Incision and Bone Removal: A surgical incision is made, and a section of the skull is removed. The size of the removed bone flap can be larger than in a craniotomy, depending on the extent of anticipated swelling.
- Brain Access and Intervention: The neurosurgeon addresses the underlying condition, such as removing a blood clot or damaged tissue.
- Dura Closure: The dura mater (the membrane covering the brain) may be expanded with a patch to further alleviate pressure.
- Skin Closure: The scalp is closed over the defect in the skull.
When is a Craniectomy Necessary?
A craniectomy is typically performed when there is significant brain swelling (cerebral edema) or a high risk of it developing. This is often seen in cases of:
- Traumatic Brain Injury (TBI): To relieve pressure from swelling after a head injury.
- Stroke: Particularly large strokes that cause significant swelling.
- Subarachnoid Hemorrhage (SAH): To manage increased intracranial pressure following bleeding in the brain.
- Malignant Cerebral Edema: Severe brain swelling from other causes.
- Post-operative Swelling: Occasionally, if significant swelling is encountered after a craniotomy, it may be converted to a craniectomy.
Key Differences: Craniotomy vs. Craniectomy
The primary difference between craniotomy and craniectomy lies in whether the bone flap is immediately replaced. Here’s a table summarizing the key distinctions:
| Feature | Craniotomy | Craniectomy |
|---|---|---|
| Bone Flap Replacement | Immediately replaced | Not immediately replaced (delayed cranioplasty) |
| Primary Purpose | Access the brain for surgery | Decompress the brain to relieve swelling |
| Typical Indications | Tumor removal, aneurysm clipping, hematoma evacuation | Traumatic brain injury, stroke, subarachnoid hemorrhage |
| Risk of Post-operative Swelling | Low to moderate | High |
| Need for Second Surgery | Less likely (unless complications arise) | High (cranioplasty to replace the bone flap) |
Cranioplasty: Reconstructing the Skull After Craniectomy
Following a craniectomy, a cranioplasty procedure is performed to replace the missing section of the skull. This is typically done several weeks or months after the initial surgery, once the brain swelling has subsided and the patient’s condition has stabilized. The bone flap, if stored, can be used. Otherwise, a custom-made prosthesis made of materials like titanium, acrylic, or other biocompatible materials is used to cover the defect. Cranioplasty not only restores the protective function of the skull but also improves the patient’s cosmetic appearance and can enhance neurological function in some cases. Our experience suggests that patients report a significant improvement in their quality of life after cranioplasty.
Benefits of Cranioplasty
- Protection of the Brain: Restores the skull’s protective barrier against injury.
- Cosmetic Improvement: Corrects the skull defect, improving appearance.
- Neurological Function: In some cases, can improve cognitive function, motor skills, and speech.
- Psychological Well-being: Can significantly improve self-esteem and reduce anxiety associated with the skull defect.
Potential Risks and Complications
Both craniotomy and craniectomy are major surgical procedures and carry potential risks and complications, including:
- Infection: Infection at the surgical site or in the brain.
- Bleeding: Bleeding in the brain or around the surgical site.
- Blood Clots: Formation of blood clots in the legs or lungs.
- Seizures: Seizures can occur after brain surgery.
- Stroke: Damage to brain tissue due to reduced blood flow.
- Cerebrospinal Fluid (CSF) Leak: Leakage of CSF from the surgical site.
- Swelling: Brain swelling, which can be particularly problematic after a craniotomy.
- Neurological Deficits: Weakness, numbness, speech problems, or cognitive impairment.
- Anesthesia-related Complications: Reactions to anesthesia.
The specific risks and complications will vary depending on the individual patient’s condition, the underlying cause of the surgery, and the surgical technique used. It’s crucial for patients to discuss these risks with their neurosurgeon before undergoing either procedure. According to a 2024 industry report, complication rates are decreasing due to advancements in surgical techniques and neuro-monitoring.
The Role of Advanced Technology
Modern neurosurgery relies heavily on advanced technology to improve the precision and safety of both craniotomies and craniectomies. These technologies include:
- Neuronavigation: Using pre-operative MRI or CT scans to create a 3D map of the brain, allowing the surgeon to precisely locate and target specific areas.
- Intraoperative Monitoring: Monitoring brain function during surgery to minimize the risk of neurological damage.
- Endoscopy: Using small cameras to visualize the brain and surrounding structures through small incisions.
- Robotics: Assisting surgeons with complex maneuvers and improving precision.
- Microscopy: Providing magnified views of the surgical field, allowing for more precise manipulation of tissues.
Life After Surgery: Recovery and Rehabilitation
Recovery after a craniotomy or craniectomy can vary depending on the individual’s condition and the extent of the surgery. In general, patients can expect to spend several days to weeks in the hospital. Following discharge, rehabilitation may be necessary to address any neurological deficits, such as weakness, speech problems, or cognitive impairment. This may involve physical therapy, occupational therapy, and speech therapy. The recovery process also includes managing pain, preventing infection, and monitoring for any complications. Support from family and friends is crucial during this time. Leading experts in neurorehabilitation emphasize the importance of early and aggressive intervention to maximize recovery potential.
Understanding Your Options: The Path Forward
Navigating the complexities of brain surgery can be daunting, but understanding the differences between procedures like craniotomy and craniectomy is a vital first step. While both procedures involve accessing the brain, their purposes and techniques differ significantly. Craniotomy focuses on precise access and immediate reconstruction, while craniectomy prioritizes decompression in cases of severe swelling. The choice between these procedures depends on the patient’s specific condition, the underlying cause of the surgery, and the neurosurgeon’s assessment. By understanding the nuances of each procedure, patients can engage in informed discussions with their medical team and make well-informed decisions about their care. If you or a loved one is facing brain surgery, it is crucial to consult with an experienced neurosurgeon to determine the most appropriate course of treatment. Explore our advanced guide to neurological conditions to learn more and empower yourself with knowledge.
