Decoding Bladder Wall Thickening: ICD-10 Codes, Causes, and Comprehensive Insights
Bladder wall thickening, a condition identified through imaging and often prompting further investigation, can be a source of significant anxiety. Understanding the potential causes, diagnostic pathways, and the role of ICD-10 codes is crucial for both patients and healthcare providers. This comprehensive guide aims to provide a detailed exploration of bladder wall thickening, its associated ICD-10 codes, the diagnostic process, potential causes, and management strategies. We strive to offer unparalleled clarity and empower you with the knowledge necessary to navigate this complex medical landscape.
Understanding Bladder Wall Thickening and ICD-10 Coding
Bladder wall thickening, also known as bladder wall hypertrophy, refers to an abnormal increase in the thickness of the bladder wall. This thickening is typically detected during imaging studies such as cystoscopy, CT scans, or ultrasounds. The significance of bladder wall thickening lies in its potential to indicate underlying conditions, ranging from benign to malignant. Accurately identifying and coding these conditions is essential for proper diagnosis, treatment, and epidemiological tracking.
ICD-10, or the International Classification of Diseases, Tenth Revision, is a globally recognized diagnostic coding system used to classify and code diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. In the context of bladder wall thickening, ICD-10 codes are used to specify the underlying cause of the thickening. Because bladder wall thickening is a finding, not a disease, there isn’t a single ICD-10 code for it. Rather, the underlying conditions that *cause* the thickening are coded.
The most relevant ICD-10 codes relate to conditions like:
- N32.89: Other specified disorders of bladder. This code could be used if the thickening is related to a specific bladder disorder not otherwise classified.
- N30 (various subcodes): Cystitis. Chronic inflammation of the bladder can lead to thickening.
- C67 (various subcodes): Malignant neoplasm of bladder. Bladder cancer is a critical consideration.
- D41.4: Neoplasm of uncertain behavior of bladder. This is used when a growth is present, but its behavior (benign vs. malignant) is not yet determined.
- R33.9: Retention of urine, unspecified. Chronic urinary retention can cause bladder wall thickening due to increased pressure.
It’s important to note that the specific ICD-10 code assigned will depend on the physician’s clinical judgment and the results of diagnostic tests. The physician must determine the underlying cause of the bladder wall thickening before assigning a final ICD-10 code.
The Diagnostic Process: Identifying the Cause of Bladder Wall Thickening
When bladder wall thickening is detected, a thorough diagnostic workup is necessary to determine the underlying cause. This process typically involves a combination of:
- Medical History and Physical Examination: The doctor will ask about your symptoms, medical history, and any risk factors you may have. A physical exam may also be performed.
- Urinalysis and Urine Culture: These tests help detect infection or blood in the urine.
- Cystoscopy: A cystoscopy involves inserting a thin, flexible tube with a camera attached (cystoscope) into the bladder to visualize the bladder lining directly. This allows the doctor to identify any abnormalities, such as tumors or inflammation.
- Imaging Studies: Imaging tests, such as CT scans, MRI scans, or ultrasounds, can provide detailed images of the bladder and surrounding structures. These tests can help identify the extent of the thickening and any other abnormalities.
- Biopsy: If a suspicious area is identified during cystoscopy, a biopsy may be performed. A small tissue sample is taken and examined under a microscope to determine if cancer cells are present.
The information gathered from these tests will help the doctor determine the cause of the bladder wall thickening and develop an appropriate treatment plan.
Potential Causes of Bladder Wall Thickening
Bladder wall thickening can result from various underlying conditions. Some of the most common causes include:
- Bladder Cancer: This is one of the most serious causes of bladder wall thickening. Cancerous tumors can invade the bladder wall, causing it to thicken.
- Cystitis: Chronic inflammation of the bladder, often caused by infection, can lead to thickening of the bladder wall over time. Both bacterial and interstitial cystitis can contribute.
- Benign Tumors: Non-cancerous growths in the bladder, such as papillomas, can also cause thickening.
- Urinary Retention: When the bladder is unable to empty completely, the chronic over-distension can lead to thickening of the bladder wall muscle. This can be due to prostate enlargement (in men), neurological conditions, or other obstructions.
- Bladder Outlet Obstruction: Any blockage in the flow of urine out of the bladder can cause the bladder muscles to work harder, leading to thickening.
- Amyloidosis: In rare cases, amyloid deposits can accumulate in the bladder wall, causing it to thicken.
- Schistosomiasis: This parasitic infection, common in some parts of the world, can cause bladder inflammation and thickening.
The Role of Cystoscopy in Diagnosing Bladder Wall Thickening
Cystoscopy stands out as a pivotal diagnostic tool when bladder wall thickening is suspected or detected through other imaging modalities. Its direct visualization capabilities offer unparalleled insights into the bladder’s internal structure, allowing for a comprehensive assessment of the thickening’s characteristics and extent. During cystoscopy, a urologist inserts a thin, flexible tube equipped with a camera (the cystoscope) into the urethra and advances it into the bladder. This procedure allows for real-time observation of the bladder lining, enabling the identification of any abnormalities, including:
- Tumors or Growths: Cystoscopy can detect the presence of tumors or growths on the bladder wall, which may be contributing to the thickening.
- Inflammation or Irritation: The procedure can reveal signs of inflammation or irritation in the bladder lining, potentially indicating cystitis or other inflammatory conditions.
- Ulcerations or Lesions: Cystoscopy can identify any ulcerations or lesions on the bladder wall that may be associated with the thickening.
- Foreign Bodies: In some cases, foreign bodies in the bladder can cause irritation and thickening of the bladder wall, which can be detected during cystoscopy.
Furthermore, cystoscopy allows for the collection of tissue samples (biopsies) from suspicious areas for further examination under a microscope. This is crucial for determining whether the bladder wall thickening is due to benign conditions or cancerous growths.
Advanced Imaging Techniques for Assessing Bladder Wall Thickening
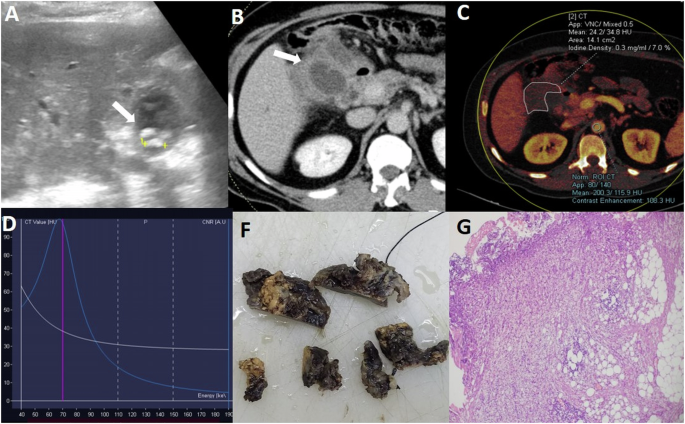
While cystoscopy offers direct visualization, advanced imaging techniques play a crucial role in providing a more comprehensive understanding of bladder wall thickening. These techniques can help determine the extent of the thickening, identify any involvement of surrounding tissues, and guide treatment planning. Several advanced imaging modalities are commonly used:
- Computed Tomography (CT) Scan: CT scans use X-rays to create detailed cross-sectional images of the bladder and surrounding structures. They can help identify the extent of bladder wall thickening, detect any masses or tumors, and assess for spread to nearby lymph nodes or organs.
- Magnetic Resonance Imaging (MRI): MRI uses strong magnetic fields and radio waves to produce high-resolution images of the bladder. MRI is particularly useful for evaluating the depth of tumor invasion into the bladder wall and assessing for spread to surrounding tissues.
- Ultrasound: Ultrasound uses sound waves to create images of the bladder. It is a non-invasive and relatively inexpensive imaging technique that can be used to assess bladder wall thickness and detect any masses or abnormalities.
- Positron Emission Tomography (PET) Scan: PET scans use a radioactive tracer to detect areas of increased metabolic activity, which can indicate the presence of cancer. PET scans are often used in conjunction with CT scans (PET/CT) to provide a more comprehensive assessment of bladder cancer.
The choice of imaging modality will depend on the individual patient’s clinical situation and the information needed to make an accurate diagnosis and treatment plan.
Treatment Strategies for Bladder Wall Thickening
The treatment for bladder wall thickening depends entirely on the underlying cause. Therefore, accurate diagnosis is paramount. Here’s a breakdown of potential treatment approaches based on common causes:
- Bladder Cancer: Treatment options may include surgery (e.g., transurethral resection of bladder tumor – TURBT, cystectomy), chemotherapy, radiation therapy, and immunotherapy. The specific approach depends on the stage and grade of the cancer.
- Cystitis: Bacterial cystitis is typically treated with antibiotics. Interstitial cystitis management involves pain management strategies, bladder training, and medications to reduce inflammation.
- Benign Tumors: Small, non-cancerous tumors may be monitored. Larger tumors may be removed surgically, often via TURBT.
- Urinary Retention/Bladder Outlet Obstruction: Treatment focuses on relieving the obstruction. This may involve medications to relax the prostate (e.g., alpha-blockers), surgery to remove prostate tissue (e.g., TURP), or intermittent catheterization to empty the bladder.
- Schistosomiasis: This is treated with antiparasitic medications.
In some cases, lifestyle modifications, such as increasing fluid intake and avoiding bladder irritants (e.g., caffeine, alcohol), may be recommended to help manage symptoms.
UroNav Fusion Biopsy: A Cutting-Edge Diagnostic Tool
UroNav fusion biopsy represents a significant advancement in the diagnosis of bladder cancer and other bladder abnormalities. This technique combines real-time ultrasound imaging with pre-acquired MRI images to create a detailed 3D map of the bladder. This fusion allows urologists to precisely target suspicious areas identified on MRI during a biopsy, increasing the accuracy of the diagnosis. Here’s how it works:
- MRI Acquisition: The patient undergoes an MRI scan of the bladder to identify any suspicious lesions or areas of concern.
- Image Fusion: The MRI images are then fused with real-time ultrasound images obtained during the biopsy procedure.
- Targeted Biopsy: Using the fused images as a guide, the urologist can precisely target the suspicious areas identified on MRI and obtain tissue samples for analysis.
UroNav fusion biopsy offers several advantages over traditional biopsy techniques, including:
- Improved Accuracy: By targeting suspicious areas identified on MRI, UroNav fusion biopsy can improve the accuracy of the diagnosis.
- Reduced False Negatives: The targeted approach can help reduce the risk of missing cancerous lesions, leading to fewer false negatives.
- Enhanced Detection of Aggressive Cancers: UroNav fusion biopsy can improve the detection of aggressive cancers, allowing for earlier treatment and better outcomes.
While UroNav fusion biopsy is a promising diagnostic tool, it’s important to note that it is not suitable for all patients. The decision to use UroNav fusion biopsy will depend on the individual patient’s clinical situation and the urologist’s judgment.
The Critical Role of Regular Checkups
Even after treatment for bladder wall thickening or any associated condition, regular follow-up appointments with a urologist are crucial. These checkups typically involve a combination of:
- Physical Examination: The doctor will perform a physical exam to assess your overall health and look for any signs of recurrence.
- Urinalysis: Urine tests will be performed to check for blood or infection in the urine.
- Cystoscopy: Periodic cystoscopies may be recommended to monitor the bladder lining for any abnormalities.
- Imaging Studies: Depending on the underlying condition and treatment, imaging tests such as CT scans or MRI scans may be performed to monitor the bladder and surrounding structures.
The frequency of follow-up appointments will vary depending on the individual patient’s situation. It is essential to adhere to the recommended follow-up schedule to ensure early detection of any recurrence or complications.
Expert Insights on Managing Bladder Health
Maintaining optimal bladder health is crucial for preventing bladder wall thickening and other bladder-related problems. While some causes are unavoidable, adopting healthy lifestyle habits can significantly reduce your risk. Here are some expert-backed recommendations:
- Stay Hydrated: Drinking plenty of water helps flush out bacteria and toxins from the bladder, reducing the risk of infection.
- Empty Your Bladder Regularly: Avoid holding your urine for extended periods, as this can weaken the bladder muscles and increase the risk of infection.
- Practice Good Hygiene: Wipe from front to back after using the toilet to prevent bacteria from entering the urethra.
- Avoid Bladder Irritants: Limit your intake of caffeine, alcohol, and acidic foods, as these can irritate the bladder and worsen symptoms.
- Quit Smoking: Smoking is a major risk factor for bladder cancer. Quitting smoking can significantly reduce your risk.
- Maintain a Healthy Weight: Obesity can increase the risk of bladder problems. Maintaining a healthy weight can help improve bladder health.
- Exercise Regularly: Regular exercise can help strengthen the pelvic floor muscles, which support the bladder.
These lifestyle modifications, combined with regular checkups and prompt medical attention when symptoms arise, can contribute significantly to maintaining a healthy bladder and reducing the risk of complications.
Taking Charge of Your Bladder Health
Understanding bladder wall thickening, its potential causes, and the diagnostic process is the first step toward proactive management of your bladder health. While the information presented here provides a comprehensive overview, it is essential to consult with a qualified healthcare professional for personalized advice and treatment. Early detection and appropriate management are crucial for achieving the best possible outcomes. If you’re experiencing symptoms such as frequent urination, painful urination, blood in the urine, or pelvic pain, seek medical attention promptly. Share your questions and concerns with your doctor, and together, you can develop a plan to address your specific needs and optimize your bladder health.
