Decoding ICD-10 Code for Oral Thrush: A Comprehensive Guide
Are you searching for clarity on the ICD-10 code for oral thrush? You’ve come to the right place. This comprehensive guide provides an in-depth exploration of the ICD-10 code B37.0, designated for oral candidiasis, commonly known as oral thrush. We’ll delve into the specifics of this code, its clinical applications, and the nuances healthcare professionals need to understand for accurate diagnosis and billing. This isn’t just a definition; it’s a complete resource designed to equip you with the knowledge and understanding you need. From understanding the underlying condition to navigating the complexities of medical coding, we’ve got you covered. We aim to provide a resource that surpasses existing information, offering a blend of expert insight and practical guidance.
Understanding the ICD-10 Code for Oral Thrush (B37.0)
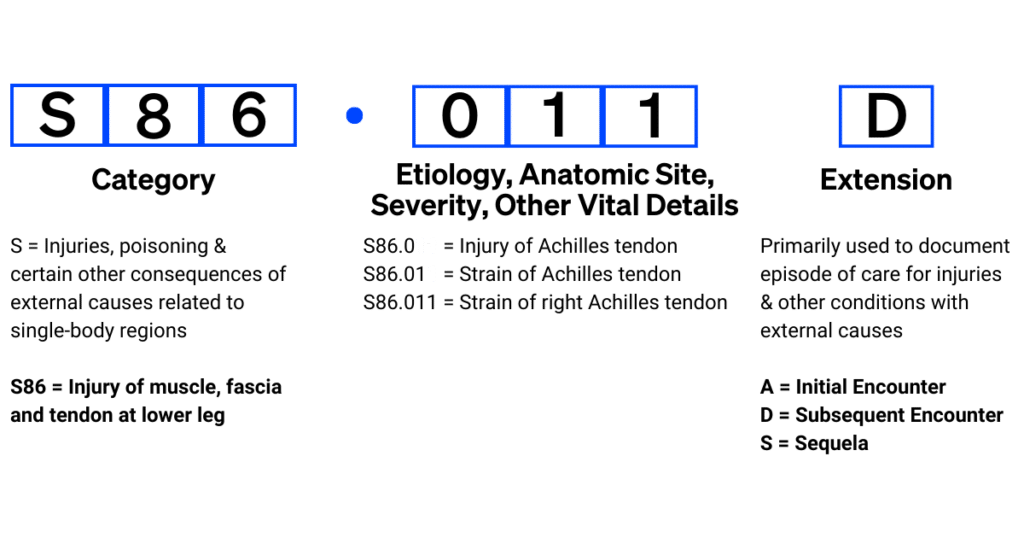
The International Classification of Diseases, Tenth Revision (ICD-10), is a globally recognized diagnostic coding system used by healthcare providers to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States. The ICD-10 code B37.0 specifically refers to oral candidiasis, more commonly known as oral thrush. This code is essential for accurate medical billing, record-keeping, and epidemiological tracking of this condition. Understanding the scope of this code requires a deeper look at what oral thrush is and how it manifests.
Oral thrush is a fungal infection caused by an overgrowth of Candida albicans, a type of yeast that naturally resides in the mouth. While Candida is usually harmless, certain conditions can disrupt the balance of microorganisms in the oral cavity, leading to an overgrowth and the development of thrush. These conditions can include weakened immune systems, antibiotic use, diabetes, and even the use of inhaled corticosteroids for asthma.
The ICD-10 system is far more detailed than its predecessor, ICD-9, allowing for greater specificity in coding. For instance, while B37 covers candidiasis, B37.0 pinpoints the infection specifically to the oral cavity. This level of detail is crucial for accurate data collection and analysis, enabling healthcare professionals to track the prevalence and incidence of oral thrush more effectively. It also allows for more precise billing processes, ensuring that healthcare providers are appropriately reimbursed for the services they provide.
Furthermore, the use of ICD-10 codes like B37.0 is vital for research purposes. By standardizing the way diseases are classified, researchers can more easily compare data across different studies and populations. This facilitates a better understanding of the risk factors, treatments, and outcomes associated with oral thrush.
Candidiasis: The Root of Oral Thrush and ICD-10 Coding
At the heart of understanding the ICD-10 code for oral thrush lies the understanding of candidiasis itself. Candidiasis, in its various forms, is a fungal infection caused by yeasts belonging to the genus Candida, with Candida albicans being the most prevalent species. While Candida is a natural inhabitant of the human body, including the mouth, gut, and skin, its overgrowth can lead to a range of infections, from superficial mucosal infections like oral thrush to invasive systemic infections.
The ICD-10 classification system recognizes the diverse manifestations of candidiasis with specific codes for each location and type of infection. For example:
- B37.0: Oral candidiasis (oral thrush)
- B37.3: Candidiasis of vulva and vagina
- B37.4: Candidiasis of other urogenital sites
- B37.5: Candidiasis of the meninges
- B37.8: Candidiasis of other sites
- B37.9: Candidiasis, unspecified
This detailed classification highlights the importance of accurately identifying the specific location of the candidiasis infection to ensure proper coding and billing. In the case of oral thrush, the presence of whitish or creamy lesions on the tongue, inner cheeks, gums, or palate is a hallmark sign. These lesions can be painful and may bleed when scraped. Patients may also experience a cottony feeling in the mouth, loss of taste, or pain while eating or swallowing.
Clinical Manifestations and Diagnosis of Oral Thrush
Recognizing the clinical manifestations of oral thrush is crucial for accurate diagnosis and subsequent coding with B37.0. Oral thrush typically presents with characteristic signs and symptoms that can be identified during a physical examination of the oral cavity. These include:
- Whitish, creamy lesions: These lesions are the hallmark of oral thrush and can appear on the tongue, inner cheeks, gums, palate, and throat. They may resemble cottage cheese and can be easily scraped off, leaving behind a red, raw surface that may bleed.
- Redness and soreness: The affected areas of the mouth may appear red and inflamed, causing discomfort or pain.
- Difficulty swallowing: In severe cases, oral thrush can extend into the esophagus, leading to difficulty swallowing (dysphagia) or a sensation of food being stuck in the throat.
- Cracking and redness at the corners of the mouth: Angular cheilitis, characterized by cracking and redness at the corners of the mouth, can sometimes accompany oral thrush.
- Cottony feeling in the mouth: Some individuals may experience a sensation of dryness or a cottony feeling in the mouth.
- Loss of taste: Oral thrush can sometimes affect the taste buds, leading to a diminished sense of taste.
While the clinical presentation of oral thrush is often sufficient for diagnosis, laboratory tests may be necessary in certain cases to confirm the diagnosis or rule out other conditions. These tests may include:
- Microscopic examination: A scraping of the oral lesions can be examined under a microscope to identify the presence of Candida organisms.
- Culture: A sample from the oral lesions can be cultured to identify the specific species of Candida causing the infection and determine its susceptibility to antifungal medications.
- Esophagoscopy: In cases where oral thrush is suspected to have spread to the esophagus, an esophagoscopy (a procedure in which a thin, flexible tube with a camera is inserted into the esophagus) may be performed to visualize the esophageal lining and obtain biopsies for further examination.
Who is Most at Risk for Developing Oral Thrush?
Certain individuals are more susceptible to developing oral thrush due to factors that disrupt the balance of microorganisms in the oral cavity or weaken the immune system. These risk factors include:
- Infants: Newborns, especially those who are breastfed, are prone to developing oral thrush due to their immature immune systems and the transfer of Candida from the mother’s nipples.
- Individuals with weakened immune systems: People with HIV/AIDS, cancer, or other conditions that compromise the immune system are at increased risk of oral thrush.
- People taking antibiotics: Antibiotics can kill beneficial bacteria in the mouth, allowing Candida to overgrow.
- People with diabetes: High blood sugar levels can create a favorable environment for Candida growth.
- People who wear dentures: Dentures can create a warm, moist environment that promotes Candida growth.
- People who use inhaled corticosteroids: Inhaled corticosteroids, used to treat asthma and other respiratory conditions, can increase the risk of oral thrush if the mouth is not rinsed after use.
- Individuals undergoing chemotherapy or radiation therapy: These treatments can weaken the immune system and increase the risk of oral thrush.
Treatment Options and Management Strategies
The treatment of oral thrush typically involves antifungal medications that target the Candida fungus. The specific treatment approach depends on the severity of the infection and the individual’s overall health. Common treatment options include:
- Topical antifungal medications: For mild to moderate cases of oral thrush, topical antifungal medications, such as nystatin suspension or clotrimazole troches, may be prescribed. These medications are applied directly to the affected areas of the mouth several times a day.
- Oral antifungal medications: For more severe or persistent cases of oral thrush, oral antifungal medications, such as fluconazole or itraconazole, may be necessary. These medications are taken by mouth and work systemically to kill the Candida fungus.
- Probiotics: Probiotics, which contain beneficial bacteria, may help restore the balance of microorganisms in the mouth and prevent Candida overgrowth.
- Good oral hygiene: Maintaining good oral hygiene, including brushing and flossing regularly, can help prevent oral thrush.
- Dietary modifications: Limiting sugary foods and drinks can help reduce the risk of Candida overgrowth.
- Addressing underlying medical conditions: Managing underlying medical conditions, such as diabetes or HIV/AIDS, can help prevent oral thrush.
The Role of Accurate ICD-10 Coding in Healthcare
Accurate ICD-10 coding is paramount in healthcare for several reasons. It directly impacts reimbursement, data analysis, and public health initiatives. Inaccurate coding can lead to claim denials, underpayment, or even legal repercussions. Furthermore, it can skew epidemiological data, making it difficult to track disease trends and allocate resources effectively.
For oral thrush, using the correct ICD-10 code (B37.0) ensures that healthcare providers are appropriately compensated for their services. It also allows for accurate tracking of the prevalence of oral thrush in different populations, which can inform public health interventions and research efforts.
Moreover, accurate coding is essential for maintaining the integrity of medical records. It provides a standardized way to document diagnoses and procedures, ensuring that healthcare providers have access to complete and reliable information about their patients. This is crucial for making informed decisions about patient care.
Related Conditions and Differential Diagnoses
While oral thrush is a distinct condition with specific characteristics, it’s important to consider other conditions that may present with similar symptoms. This process of differential diagnosis helps healthcare professionals arrive at the correct diagnosis and ensure appropriate treatment. Some conditions that may mimic oral thrush include:
- Leukoplakia: Leukoplakia is a condition characterized by white patches or plaques that develop on the mucous membranes of the mouth, including the tongue and inner cheeks. Unlike oral thrush, leukoplakia lesions are typically firmly attached and cannot be easily scraped off. Leukoplakia can be caused by chronic irritation from tobacco use, alcohol consumption, or ill-fitting dentures.
- Lichen planus: Lichen planus is an inflammatory condition that can affect the skin, mucous membranes, and nails. Oral lichen planus can present with white or lacy patches on the inner cheeks, gums, or tongue. These patches may be accompanied by redness, soreness, or burning sensations.
- Hairy leukoplakia: Hairy leukoplakia is a condition characterized by white, hairy-like patches on the sides of the tongue. It is typically caused by the Epstein-Barr virus (EBV) and is often seen in individuals with weakened immune systems, such as those with HIV/AIDS.
- Aphthous ulcers (canker sores): Aphthous ulcers are small, painful sores that can develop on the inner cheeks, gums, or tongue. Unlike oral thrush, aphthous ulcers are typically solitary and have a distinct appearance, with a red halo surrounding a white or yellowish center.
- Oral cancer: In rare cases, white or red patches in the mouth may be a sign of oral cancer. It is important to rule out oral cancer, especially if the lesions are persistent, growing, or accompanied by other symptoms, such as difficulty swallowing or speaking.
The Future of ICD-10 and Oral Thrush Coding
The ICD system is not static; it evolves to reflect advances in medical knowledge and changes in healthcare practices. While ICD-10 is currently in use, the World Health Organization (WHO) has already released ICD-11. As healthcare transitions to ICD-11, it’s crucial for professionals to stay informed about any changes that may affect the coding of oral thrush and related conditions.
The transition to ICD-11 will likely bring even greater specificity and granularity to diagnostic coding. This could potentially lead to more refined codes for different types of oral candidiasis or for oral thrush associated with specific underlying conditions. Staying updated with these changes will be essential for accurate coding, billing, and data analysis.
Navigating the Nuances of Oral Thrush Coding
In conclusion, understanding the ICD-10 code B37.0 for oral thrush is crucial for healthcare professionals involved in diagnosis, treatment, and billing. It requires a comprehensive understanding of the condition, its clinical manifestations, risk factors, and treatment options. Accurate coding ensures proper reimbursement, facilitates data analysis, and supports public health initiatives. By staying informed and adhering to best practices, healthcare professionals can contribute to improved patient care and a more efficient healthcare system. Share your experiences with ICD-10 coding for oral thrush in the comments below.
